For the purpose of this writing I am using the word “fetish” somewhat interchangeably with the word “kink”, and as a general concept rather than a medical diagnosis. “Fetish” and “kink” have separate meanings, though they are often conflated, and the degree to which something is considered a kink or fetish is personal and arguable outside of psychological evaluation. A fetish is understood to be something (often an object, objectified body part, or action) which needs to be present for someone to obtain sexual arousal and/or release. Example: a foot fetishist may not be able to orgasm or become sexually turned on without seeing, touching, or fantasizing about a person’s foot. People develop sexual fetishes for a wide variety of reasons at different points in their life, and someone with a “true” clinically diagnosed fetish is not what is generally meant when people use the word. The term fetish is frequently used to indicate a strongly enjoyed kink. The word fetish is also used to indicate kinks which reside specifically within the world of objectification: latex, shoes, nylons, feet, sissification, trans people’s bodies, women’s bodies, dick size, etc. When focus is placed on what a person is wearing, how they present, are physically formed, or something other than the integrated person themselves as reason for sexual interest, the word fetish is appropriate. Example: a person who doesn’t care what you look like as long as you’re wearing latex—that person will find you attractive because they have a latex “fetish”. A kink is a sexual taste which is considered out of the ordinary. How common or uncommon a kink actually is varies wildly. People frequently disagree about where a certain activity resides on a spectrum of vanilla to kinky. Example: spanking. Some people consider spanking to be a normal part of sexual activity and so vanilla by nature, others consider it to be kinky and not a behavior to be defined within the boundaries of an “ordinary vanilla” sexual connection.
Control of other people’s bodies is a kink which has reached fetishistic proportions in our society. Our culture’s widespread practice of objectification is a primary reason for this, which is made even more complex within a social structure where gendered privilege and unchecked entitlement runs rampant. Most people don’t consider themselves to be objectifiers, however, related behaviors and ways of thinking are so part and parcel of how we’re raised and what coping mechanisms we learn at an early age, I posit that almost everyone wrestles with these values (or is confronted with them) at some point in their life. In a capitalistic society we are held to the standards of ad campaigns and salability everywhere we look, it’s pervasive and insidious. It’s almost unavoidable not to hold our friends and family, celebrities, public figures, and even the strangers we interact with to these same standards and expectations. The alternative to reactionary objectification is practicing acceptance, curiosity, and enjoyment of a diversity of personal presentations, rather than jumping to judgement based on appearance.
It isn’t bad or evil to objectify, but it is important to gain consent when it will effect the person targeted. A “trendy” form of objectification these days is the obsession with knowing what’s contained in other people’s shorts. In conversations about sex, gender, orientation, identity, even lawmaking, and filing paperwork, an entitlement around knowing someone’s phenotypic sex characteristics outshines discussion of their character, skills, intellect, behaviors, or energetic capabilities.
That’s some pretty bullish stuff… why is it this way? I think a large part of what makes our society so concerned—even fanatic about other people’s private bodies—is in order to control their own personal branding, which is frequently expressed as an unyielding claim to a limited or stringent idea of sexual orientation. In short, we are obsessed with other people’s appearances in order to maintain the image (or belief) that we ourselves are of one sexual orientation or another. It’s commonly accepted that people lean on others to “keep up appearances” in order to telegraph a comfortable public image of themselves, based upon whom they associate with.
I was teaching a workshop about gender and sexuality recently, and in class a question was raised about how to appropriately ask after a person’s genitalia while cruising. How does one find a partner with the genitalia they are attracted to, prefer, or are interested in playing with if it’s rude to ask someone about their phenotypic sex traits? In the recent past, with the binary more firmly in place, one simply made assumptions about who they were bringing home and what the sex might be like. They were either pleased, proven wrong, or exposed to a whole new experience by the end of the evening. Nothing has really changed. If someone makes you laugh when you chat on the dance floor and you like their moves, you will still be surprised when they remove their garments and reveal the size, color, shape, stiffness, or coiffure of what they’ve got going on under all those layers. One will, of course, be even further surprised at discovery of the depth, sensitivity, solidity, strength, technique, longevity, sensual interests, texture, chemistry, scent, and experience of that individual as seduction and actual play come to pass… Nothing is certain until you’ve tasted the damn fruit.
If you’re hooking up with a relative stranger, chances are you aren’t solidly wed to complete control of what happens, with whom, or how it goes down. That’s a much surer bet within a longterm relationship. In hook-up situations people are looking to satisfy an urge in combination with the projection of a fantasy. If one is driven to connect with someone they don’t know, and with little time for interview, chances are they’re actually looking to get off however they can get it, not satisfy a deep connection with someone they respect as separate and equal. Whatever that hook up is like, chances are it’s also not going to be wholly articulated by one person’s fantasy. If that was the goal, they would have taken the time to find someone to service them properly within the boundaries of their specific desires.
When one engages in longer term or friend-first sexual connections, they certainly don’t fall in love/lust/sexual intrigue based on what their partner’s junk looks like either. Many people fall in love with their partner’s perfect groin because of how it makes them feel, because it’s connected to the person they love, and sometimes also because of how it looks. When one takes the time to get to know a person before negotiating sexual intimacy, there’s usually an emotional and/or mental connection cultivated which cannot be ignored when discussing the reasons for sex. This too is far from fetishistic.
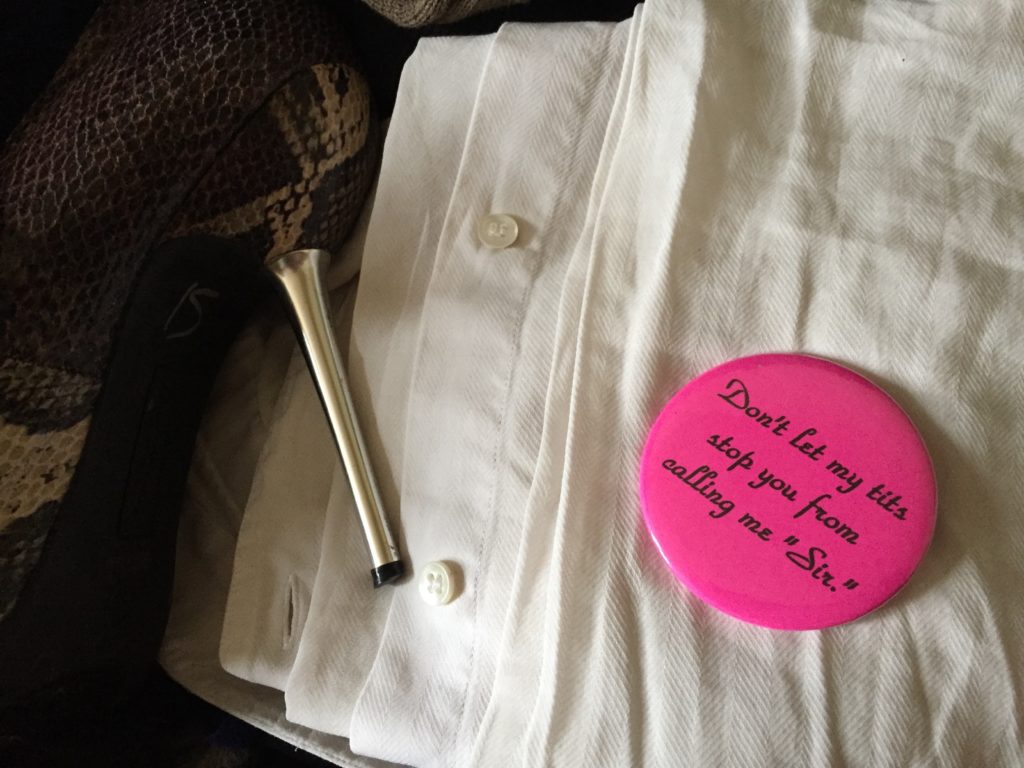
In our current age of emergent nonbinary acceptance, visibility, and public acknowledgement, in order for people to defend an unwavering sexual identity, focus on phenotypic sex traits inappropriately comes to the forefront of conversation and highlights this social anxiety. For example: if someone notices me, decides they’re attracted to me, and jumps to correspondent fantasies about what it might be like to have sex with me, that’s all very well and normal. It’s also on them and not my responsibility. That person’s fantasy has nothing to do with the actual living, breathing, autonomous me. Their assumption, i.e. wish, that I might enjoy a particular activity, or that the body under my clothes appears a certain way, or that I might respond favorably to a particular type of stimulus, is their fantasy and it has nothing to do with my actual physical, emotional, and psychological interests or lived reality. We do not generally fall for people because of the size, color, type, hairiness, or functionality of their genitalia. If one does fall for someone’s specific size, color, type, hairiness, or genital functionality, it’s very simply defined as: their fetish. It’s the responsibility of anyone harboring a fetish to negotiate their desires honestly in order to fulfill them appropriately and respectfully. It’s definitely not the object of their desire’s responsibility to fulfill those fantasies or fetishistic expectations.
While we live in a highly fetishistic society, that’s in no way an excuse to pursue controlling someone else’s body outside of their willingness to be so. If a person needs their partner to present their body in a specific way in order to enjoy intimacy, it’s their responsibility to negotiate the scenario they wish to engage in, or let it go, or move on to someone willing to play those particular games. For example: if your kink is shaved genitals, good for you. I do not shave my genitals. It’s also none of your business if I shave my genitals unless I want to share that information with you. I am probably not going to shave for you, as it’s my right to tend to my body exactly as I please, and shaving does not please me—quite the opposite. Your kink/preference/fetish doesn’t overshadow my right to keep my autonomous unshaved body as I prefer it to be. Your desire to fulfill your fantasy with me also doesn’t give you the right to demand me to reveal private information about my body. If you cannot get over this particular desire then we’ll probably not interact sexually. No big deal. If you happen to fetishize something I’m also into, we’ll probably have a lot of fun with that thing as long as you don’t objectify me about it. If you want to objectify me, that’s a separate fetish and negotiation, and I’ll probably require aftercare if I decide to engage you in that way because one of my deepest kinks and emotional needs is connection.
Back to my student’s initial question: I answered, “Taking personal responsibility for one’s desires is key to success”. Saying something to the effect of, “I’m really horny and came out tonight looking for X—is that something you’re interested in or might want to help me out with?”, is a far cry from, “do you have a pussy or a dick?”. The first sentence takes responsibility for and names a specific personal desire, and then asks if there’s mutual interest in further conversation about it. It allows the person being asked to respond in a number of ways based on what they’re comfortable revealing. That person might simply say, “No thanks”, or they might mention they can’t physically fulfill the desire expressed, or maybe they’ll check in about toy use or alternative hole penetration in lieu of specific biological requests, or maybe they’ll even reveal their own desires so the discussion can build into something more mutually agreeable… the options are limitless. The second question indicates an entitlement to knowledge about someone else’s private body. It also implies an assumption that if the person answers “correctly”, that there’s an interest in engagement, and so puts a responsibility of rejection and/or clarification on the person being asked. Further, it assumes that having a particular physical trait equals a desire to engage that physicality in a specific way during sexual congress. None of these assumptions or implications respect another person’s values, skills, availabilities, psychology, history, potential traumas, or interests.
Fetishes can be wonderful, and my argument is not to draw the conclusion that one should do away with such things—even objectification. What I think we need to get better at is practicing communication about and gaining consent for our fetishistic desires, rather than bullying people by way of shame, negging, abuse, neglect, unasked for behavior modifications, games, and guilt trips in order to repress them, convince them to conform, or otherwise control their actions and bodies outside of their personal values and interests. If you’re completely disinterested in becoming involved with a person who has a particular style of genitalia, it’s your responsibility to be honest and upfront about that before unduly wasting the time and energy of the person you’ve approached. It’s never the job of those you flirt with to preemptively let you know anything about their bodies, as if their bodies might be potentially “wrong”, or as if their bodies exist primarily to be pleasing to you. When we can better navigate our own fetishistic interests, we may even find ourselves more excited about and equipped to satisfy other people’s interests as well.
If you’re interested in more conversation about gender, kink, sexual behavior, BDSM skills, or similar subjects, please contact me about presenting at your party, convention, school, or event. I love teaching theory and practical skills, and I enjoy developing new curriculum to suit my client’s needs. Alternatively, if you’d like to support my work, research, travel, writing, and other artistic creations please join my Patreon campaign. Thanks.
Play On My Friends,
~ Creature
This writing takes time, research, and consideration. It is my art.
Please visit my Patreon, offer one time Support or email me for other options. Thank you.

